Abstract
Background. HPgV (previously called GBV-C) is a single-stranded RNA virus belonging to the Flaviviridae, and is the most closely related human virus to the Hepatitis C virus. HPgV is transmitted through parenteral, sexual and perinatal routes and replicates in vitro in T and B-lymphocytes. Active infection lasts months to years and viremia can be detected in plasma by real time (RT)-PCR methods. HPgV viremia has been linked to risk of non-Hodgkin lymphoma in some previous studies, but these have had a limited number of cases. In the largest study conducted to date, we evaluated the association of HPgV viremia and viremic load (VL) with risk of developing lymphoma, overall and by major subtypes, in the Mayo Clinic Case-Control Study of Lymphoma. Because the virus has also been associated with better prognosis in the setting of co-infection with HIV in many studies, we further assessed the association of HPgV with prognosis. Finally, to better understand the association of HPgV with lymphoma risk we correlated the HPgV status with circulating levels of selected cytokines in a subset of our controls.
Methods. To assess the role of HPgV in lymphoma risk (etiology), we used risk factor data and banked plasma samples (stored at -80°C) from 2094 lymphoma cases newly diagnosed from 2002-2009 and 1572 frequency matched controls. Plasma samples (blind to case/control status) were tested for HPgV RNA by RT-PCR, and those with RNA concentrations < 5,000 genome equivalents/ml were confirmed using nested RT-PCR methods. We used unconditional logistic regression model to estimate odds ratio (ORs) and 95% confidence intervals (CI) for the association of HPgV status (negative/positive) and VL (tertiles among positive controls) with lymphoma risk, adjusted for age and sex. To assess the role of HPgV in lymphoma outcome (prognosis), we used 2948 cases from the Iowa/Mayo Molecular Epidemiology Resource, a prospective cohort study of newly diagnosed lymphoma patients (included all cases from the case-control study). We used Cox proportional hazards regression models to estimate hazard ratios (HRs) and 95% CI for the association of HPgV viremia status and VL with event-free (EFS) and overall (OS) survival, adjusted for clinical and treatment variables. Circulating serum cytokines in 379 controls with HPgV data were analyzed using the Luminex-100 system Version 1.7. Data were acquired using STar Station software and analysis was performed using the MasterPlex QT 1.0 system.
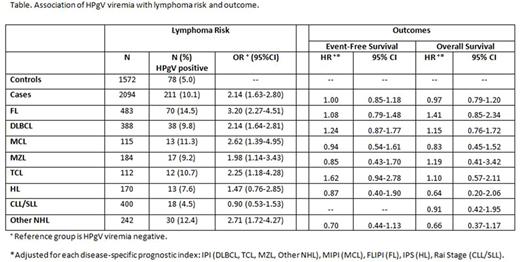
Results. The mean age of cases was 61 years, and 58.2% were male, while the mean age of controls was 63 years, and 51.1% were male; 78 (5.0%) controls and 211 (10.1%) cases were HPgV positive. There was a positive association of HPgV viremia with risk of lymphoma overall (OR = 2.14; 95% CI 1.63-2.80; p <0.0001), and for all major subtypes except HL and CLL/SLL (Table). Further adjustment for history of hepatitis, transfusion, autoimmune disease, atopy, family history of lymphoma, farming, obesity, smoking, alcohol use, or sun exposure did not confound these results, and results were consistent when excluding plasma samples (38%) collected after initiation of treatment. There was no dose-response association of VL with overall lymphoma risk: compared to HPgV negative, OR = 1.8 for lowest tertile (95% CI 0.58-5.97), OR = 4.3 for middle tertile (95% CI 0.97-19.6), and OR = 2.5 for highest tertile (95% CI 0.95-6.97). In the control group, median levels of serum sIL2-R (p=0.04), MIP1α (p=0.03) and MIG (p=0.02) were significantly higher in HPgV viremia positive compared to HPgV negative controls. In contrast to the analysis for risk, there was no association of HPgV viremia with EFS (HR = 1.00; 95% CI 0.85-1.18) or OS (HR = 0.97; 95% CI 0.79-1.20) for lymphoma overall, nor for any of the subtypes (Table). Likewise, there was no association of EFS or OS with viremic load.
Conclusion. HPgV infection was associated with the overall risk of lymphoma, as well as most of the major NHL subtypes except CLL/SLL and HL, and this was not confounded by other lymphoma risk factors. However, there was no association of HPgV status with prognosis. Among controls, HPgV viremia was associated with higher levels of IL-2R, MIP1α and MIG, which were previously associated with risk of DLBCL and FL in a case-control analysis, and suggests potential mechanistic pathways for further exploration. These data support the hypothesis for a role for this virus in the etiology of multiple lymphoma subtypes.
Nowakowski: Nanostring: Research Funding; Bayer: Consultancy, Research Funding; Abbvie: Consultancy; Genetech: Consultancy, Research Funding; Morphosys: Consultancy, Research Funding; celgene: Consultancy, Research Funding; pharmacyclics: Consultancy. Ansell: Affimed: Research Funding; Seattle Genetics: Research Funding; Bristol-Myers Squibb: Research Funding; Merck: Research Funding; Celldex: Research Funding. Cerhan: Janssen: Other: Scientific Advisory Board (REMICADELYM4001); Janssen: Other: Multiple Myeloma Registry Steering .
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal